Behind the Rejections: An Analysis of 89 FDA CRLs Reveals Why Drugs Really Fail to Get Approved
We take a look at the newly released Complete Response Letters that expose the systematic barriers preventing new drugs from reaching patients.
Only paid subscribers get regular full access to our guidance breakdowns and other analyses. If you’re not already a paid subscriber, you can upgrade here.
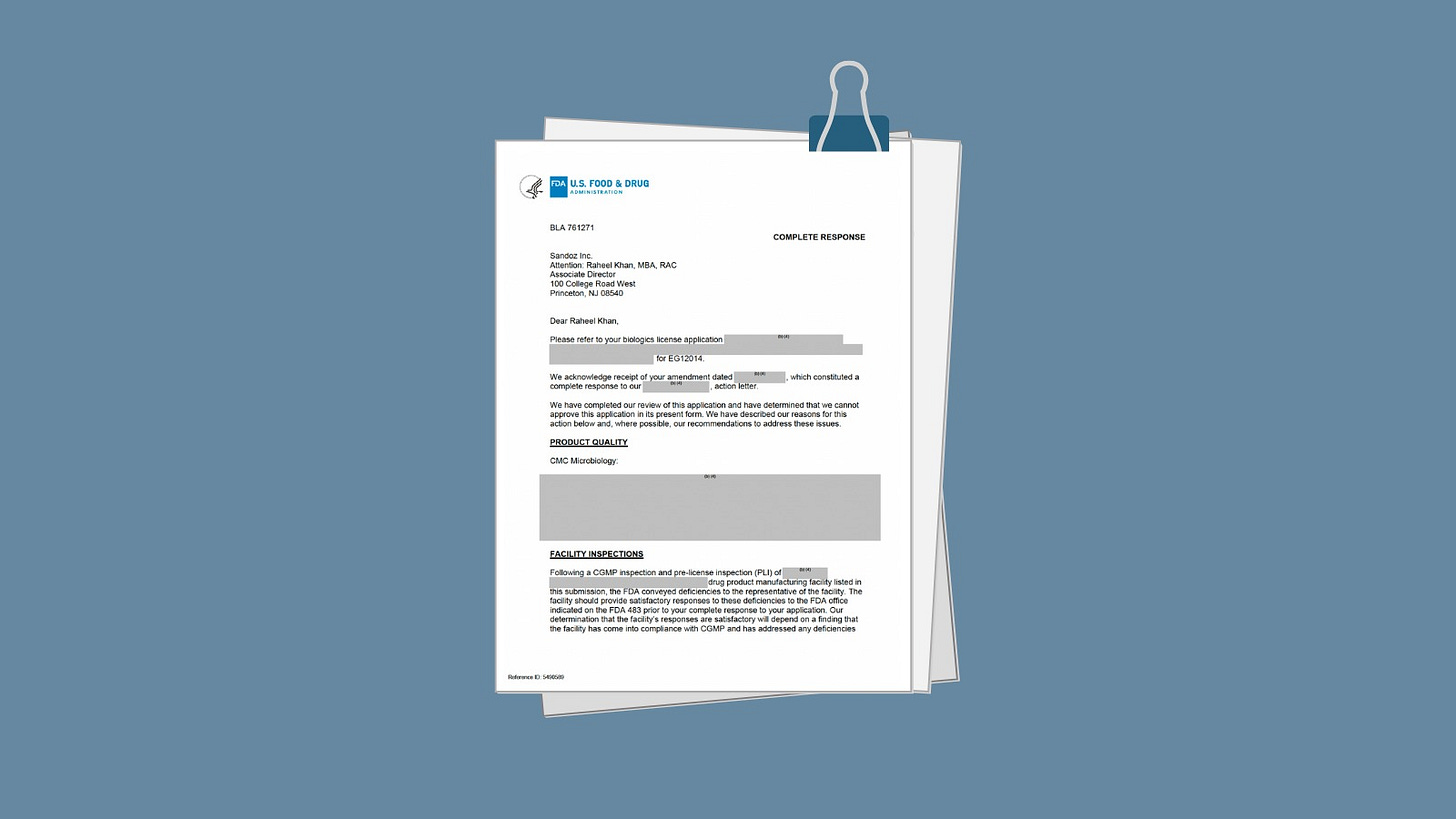
Last week, the FDA made an unprecedented move toward transparency by releasing 89 Complete Response Letters (CRLs) for products that have not been approved—documents that until now have remained largely hidden from public view.
Unlike the previous batch of 200+ CRLs for already-approved products, these letters provide an unvarnished (although heavily redacted) look at why therapies fail at the final regulatory hurdle. Notably, this release includes CRLs from both CDER and CBER, providing the first real view across the FDA's drug and biologics centers.
FDA Commissioner Martin Makary announced that going forward, the agency will "promptly release newly issued CRLs" with appropriate redactions, marking a new era of regulatory transparency.
But what do these documents actually tell us about the state of drug development and approval in 2025?
We conducted an exhaustive analysis of all 89 CRLs, all issued between January 2024 and January 2025. Our findings not only paint a sobering picture of the challenges facing drug developers but also validate the concerning patterns our consultants have been observing in the field for the past two years.
At a high level, our analysis reveals three dominant categories of deficiencies:
56% (50/89) contain facility inspection-related approvability issues.
47% (42/89) cite product quality deficiencies.
Over 30% (29/89) include clinical or clinical/statistical failures.
These aren't mutually exclusive. Many CRLs contain multiple categories of deficiencies, suggesting systemic preparation failures rather than isolated problems.
Let’s break this down.
Facility inspection issues (most common—56% of all CRLs)
The dominance of facility inspection issues (56% of all CRLs) confirms what our own mock inspection teams most commonly put in their reports (and help teams work on). Sometimes these are minor documentation gaps, but as these numbers reveal, there’s a surprising number of fundamental failures in CGMP compliance.
This is the pattern we tend to see here that drives into this problem:
FDA inspectors issue Form 483 observations during facility inspections for CGMP problems.
Companies provide responses they believe address the issues.
The FDA determines that the corrections are insufficient to address the "systemic issues."
Re-inspection is required, often multiple times.
The product cannot be approved until manufacturing compliance is verified.
One particularly telling example comes from multiple CRLs where the FDA explicitly states that corrective actions "do not appear to be comprehensive enough to address the systemic issues observed during the inspection." The word "systemic" appears repeatedly—this isn't about isolated problems but baseline flaws in quality systems.
The inclusion of CBER CRLs reveals that biologics manufacturers face even steeper challenges. Multiple CBER CRLs cite facilities requiring "additional review and verification during a subsequent inspection"—language that typically means 12-18 months of delay.
We often advise biologics firms to start facility preparation at Phase 1, not Phase 2. For cell and gene therapies, our consultants recommend running quarterly mock inspections beginning 24 months before BLA submission. The complexity of biologics manufacturing means traditional timelines are mostly obsolete, but many firms still need to realize this.
Product quality (47% of CRLs)
While clinical failures get headlines, product quality issues lurk in nearly half of all CRLs—and these details are almost entirely redacted, making them invisible to outside observers until now.
The heavy redaction of product quality sections initially frustrated our analysis, but our consultants recognize these patterns from our client engagements and can attempt to (anecdotally) fill in the black boxes.
Common product quality failures we're seeing include:
Analytical method validation inadequacies.
Stability data gaps or failures.
Specifications not justified by development data.
Process validation is incomplete or flawed.
Container closure integrity issues.
Extractables/leachables studies are insufficient.
In the words of one of our clinical quality consultants:
The redactions actually tell us something important: the FDA is protecting proprietary manufacturing details, but the pattern is clear—companies are submitting applications with fundamental chemistry, manufacturing, and controls gaps they assumed the FDA wouldn't catch (or failed to catch themselves).
One recent firm came to us after receiving a CRL citing "inadequate analytical method validation"—seemingly a straightforward fix. Our CMC team's investigation revealed:
7 analytical methods requiring complete revalidation.
Invalid methods compromised 18 months of stability data.
Several million dollars in additional costs to remediate.
2-year delay to approval.
This is why we always suggest firms engage an independent CMC review at least 18 months before submission.